Hemolyzed Blood Explained
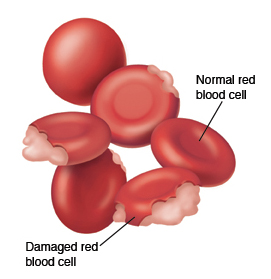
Hemolyzed blood is blood that has undergone hemolysis, which is the process of breaking down or destroying red blood cells. Hemolysis can occur for a variety of reasons, and can have significant implications for the patient’s health.
Red blood cells contain a pigment called hemoglobin, which is responsible for carrying oxygen from the lungs to the body’s tissues. When red blood cells are healthy and functioning properly, they are able to transport oxygen efficiently, helping to maintain the body’s vital functions.
However, when red blood cells are damaged or destroyed, they can release their hemoglobin into the bloodstream, resulting in hemolyzed blood. Hemolyzed blood is typically characterized by a reddish-brown or yellowish color, and may have a distinct, unusual smell.
Why Does Hemolysis Occure?
Hemolysis can occur for a variety of reasons, including:
Physical trauma: Red blood cells can be damaged or destroyed if they are subjected to physical trauma, such as being struck by a high-velocity object or being crushed by a tight-fitting bandage or other medical device.
Infections: Some infections, particularly those caused by certain types of bacteria, can damage or destroy red blood cells.
Autoimmune disorders: Some autoimmune disorders, such as sickle cell anemia, can cause the body’s immune system to attack and destroy its own red blood cells.
Medications: Some medications, such as certain antibiotics and chemotherapy drugs, can cause hemolysis by damaging or destroying red blood cells.
Hemolyzed blood can be a serious health concern, as it can disrupt the body’s ability to transport oxygen and may lead to a variety of complications. If you have any concerns about hemolyzed blood or other aspects of your health, it is important to speak with a healthcare professional for further evaluation and treatment.
Blood Tests For Hemolysis
There are several different blood tests that can be used to detect hemolysis, or the breakdown of red blood cells. These tests can help healthcare professionals diagnose and treat conditions that may be causing hemolysis, and can help monitor the effectiveness of treatment.
Some common blood tests that may be used to detect hemolysis include:
Complete blood count (CBC): A CBC is a routine blood test that measures the number and characteristics of different types of blood cells, including red blood cells. A CBC can help healthcare professionals detect hemolysis by looking for abnormal levels of red blood cells or other indicators of red blood cell damage or destruction.
Blood smear: A blood smear is a laboratory test that involves examining a sample of blood under a microscope. During a blood smear, a healthcare professional will look for abnormal red blood cells or other indicators of hemolysis, such as red blood cells that are misshapen or have abnormal colors or shapes.
Blood chemistry panel: A blood chemistry panel is a laboratory test that measures the levels of various chemicals in the blood, including enzymes and other substances that are released when red blood cells are damaged or destroyed. An abnormal blood chemistry panel may be a sign of hemolysis.
Lactate dehydrogenase (LDH) test: The LDH test is a laboratory test that measures the levels of an enzyme called lactate dehydrogenase in the blood. LDH is released when red blood cells are damaged or destroyed, and an elevated LDH level may be a sign of hemolysis.
Reticulocyte count: A reticulocyte count is a laboratory test that measures the number of reticulocytes in the blood. Reticulocytes are immature red blood cells that are produced in response to a shortage of red blood cells. An elevated reticulocyte count may be a sign of hemolysis.
These are just a few of the blood tests that may be used to detect hemolysis. If you have any concerns about hemolysis or other aspects