In the realm of medical treatments and procedures, there exists a lesser-known acronym, ORIF. This abbreviation stands for Open Reduction Internal Fixation, a surgical technique utilized to treat fractures that cannot be successfully mended through casting or splinting alone. Driven by our unwavering commitment to providing accurate and reliable health information, we aim to shed light on the intricacies of the ORIF medical procedure. By delving into the details, we hope to empower individuals with a deeper understanding of this intricate surgical intervention.

What is ORIF?
Definition
ORIF stands for Open Reduction Internal Fixation. It is a surgical procedure used to treat fractures, dislocations, birth defects, and osteoporosis-related bone fractures. ORIF involves making an incision to access the fractured bone, realigning the bone fragments, and then securing them using internal devices such as metal plates, screws, or rods. This procedure aims to restore the normal anatomical alignment of the bone and promote proper healing.
Purpose
The main purpose of ORIF is to restore the normal function and alignment of fractured bones or joints. By stabilizing the fractured bone with internal fixation devices, ORIF allows for proper healing and decreases the risk of long-term complications such as deformity, impaired mobility, and chronic pain. Additionally, ORIF can reduce the risk of complications associated with prolonged immobilization, such as muscle atrophy and joint stiffness. The ultimate goal of ORIF is to facilitate a successful recovery and restore the patient’s quality of life.
Reasons for ORIF
Fractures
One of the primary reasons for performing ORIF is to treat fractures. Fractures can occur in various bones throughout the body, such as the arms, legs, pelvis, or spine. Complex fractures, open fractures (where the broken bone punctures the skin), or fractures that involve multiple bone fragments may require surgical intervention like ORIF. This procedure helps to stabilize the bone fragments and promote proper healing.
Dislocations
In cases where a joint becomes dislocated, ORIF may be necessary to restore proper alignment. Dislocations occur when the ends of bones in a joint are forced out of their normal positions. This can result in pain, swelling, and impaired function of the joint. ORIF can be used to realign and stabilize the joint, allowing for the proper healing of ligaments and tissues surrounding the joint.
Birth defects
In some cases, individuals may be born with certain bone deformities or birth defects. ORIF can be utilized to correct these abnormalities and improve the function and appearance of the affected area. This may involve realigning bones, removing excessive growth, or using internal fixation devices to stabilize the area.
Osteoporosis
Osteoporosis is a medical condition characterized by weakened and brittle bones, making them more susceptible to fractures. When individuals with osteoporosis experience a fracture, ORIF may be necessary to stabilize the bone and promote proper healing. This procedure can help reduce pain, restore function, and prevent further fractures in individuals with osteoporotic bones.
Preparation for ORIF
Medical evaluation
Prior to undergoing ORIF, a comprehensive medical evaluation is necessary. This evaluation involves a detailed examination of the patient’s overall health, medical history, and any pre-existing conditions that may affect the surgery or recovery. The healthcare team will also order diagnostic tests, such as X-rays or CT scans, to gain a better understanding of the specific nature and extent of the fracture or condition.
Patient counseling
Patient counseling is an important part of the ORIF preparation process. The healthcare team will educate the patient about the procedure, its risks, benefits, and expected outcomes. They will also discuss alternative treatment options and address any concerns or questions the patient may have. Proper communication and understanding are crucial to ensure that the patient is well-informed and mentally prepared for the upcoming surgery.
Medication instructions
Prior to the ORIF procedure, the patient may be given specific medication instructions. This may include discontinuing certain medications that can increase the risk of bleeding or interfere with the anesthesia. In some cases, the patient may be prescribed prophylactic antibiotics to minimize the risk of infection. It is essential for the patient to follow these instructions carefully and inform the healthcare team about any existing medications or allergies.
Surgical planning
Surgical planning plays a vital role in the success of ORIF. The healthcare team will carefully assess the nature of the fracture or condition and plan the surgical approach accordingly. This includes determining the appropriate type and size of internal fixation devices, as well as discussing the specific surgical technique that will be used. Preoperative imaging studies and discussions amongst the surgical team help ensure optimal planning and preparation for the procedure.
The ORIF Procedure
Anesthesia
During the ORIF procedure, anesthesia is administered to ensure the patient’s comfort and safety. The type of anesthesia used depends on various factors, including the patient’s overall health, the extent and location of the fracture, and the surgeon’s preference. General anesthesia may be used, which will render the patient unconscious throughout the surgery. Alternatively, regional or local anesthesia may be employed to numb only the specific area being operated on.
Incision
Once the patient is anesthetized, the surgeon will make an incision to access the fractured bone or joint. The location and length of the incision depend on the specific fracture and the surgical approach chosen. The surgeon will carefully create an incision that provides optimal visibility and access to the fracture site while minimizing damage to surrounding tissues.
Fracture Reduction
After making the incision, the surgeon will proceed with the fracture reduction. This involves realigning the bone fragments to their normal anatomical position. Various techniques may be used to achieve fracture reduction, such as manual manipulation, traction, or the assistance of specialized instruments. The surgeon will carefully evaluate the alignment of the bone fragments using imaging guidance during this process.
Fixation
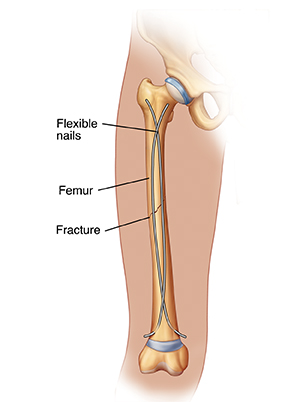
Following fracture reduction, the surgeon will utilize internal fixation devices to stabilize the bone and promote proper healing. These devices may include metal plates, screws, nails, rods, or wires, which are carefully positioned and affixed to the bone to maintain its alignment. The specific choice and placement of these devices depend on the nature of the fracture and the surgeon’s judgment.
Closure
Once the fracture has been stabilized with internal fixation devices, the surgeon will proceed to close the incision. This is typically done using absorbable or non-absorbable sutures or staples. The closure technique aims to provide adequate wound healing while minimizing scarring. In some cases, a sterile dressing or surgical adhesive may be applied to the incision site to protect it during the initial recovery period.

After ORIF Surgery
Recovery Room
After the ORIF procedure is completed, the patient is moved to the recovery room, where their vital signs and overall condition are monitored closely. The recovery room staff will ensure that the patient is awake, stable, and recovering well from anesthesia. This is a critical period during which the patient’s pain levels, blood pressure, heart rate, and respiratory function will be closely observed.
Pain Management
Managing postoperative pain is an important aspect of the recovery process following ORIF surgery. The healthcare team will provide appropriate pain medications to ensure the patient’s comfort. These may include opioids, non-steroidal anti-inflammatory drugs (NSAIDs), or local anesthetics. Effective pain management not only enhances the patient’s comfort but also promotes early mobilization and rehabilitation.
Physical Therapy
Physical therapy plays a significant role in the recovery phase after ORIF surgery. The patient will work closely with a physical therapist to regain strength, flexibility, and functionality in the affected area. The physical therapist will design a tailored rehabilitation program that includes exercises and activities aimed at improving movement, reducing stiffness, and promoting the healing process. Regular physical therapy sessions are crucial for maximizing the patient’s recovery and restoring pre-injury function.
Follow-up Care
Following ORIF surgery, regular follow-up visits with the healthcare team are essential. These visits allow the surgeon to assess the progress of healing, remove any sutures or staples, monitor the patient’s range of motion and functionality, and address any concerns or complications that may arise. The frequency and duration of follow-up care depend on the specific case and the surgeon’s recommendation.
Risks and Complications
Infection
Infection is a potential complication following ORIF surgery. The surgical incision creates an entry point for bacteria, increasing the risk of infection in the underlying bone or surrounding tissues. Prophylactic antibiotics are often administered to reduce this risk. However, if an infection does occur, it may require additional treatment such as antibiotic therapy or, in severe cases, surgical intervention to drain the infected area.
Bleeding and Blood Clots
During ORIF surgery, there is a risk of bleeding due to damage to blood vessels. While surgeons take precautions to minimize bleeding, some patients may experience excessive or prolonged bleeding. Blood clots, known as deep vein thrombosis (DVT), can also occur after surgery, especially in the lower extremities. Measures such as early mobilization, compression stockings, and blood-thinning medications may be employed to reduce the risk of blood clots.
Nerve Damage
Nerve damage is another potential risk associated with ORIF surgery. Manipulating or repositioning fractured bones can put nearby nerves at risk of injury. This can result in temporary or permanent sensory or motor deficits, such as numbness, weakness, or tingling. Surgeons take great care to minimize the risk of nerve damage during surgery, but it is an inherent risk associated with any surgical procedure involving delicate structures.
Implant Failure
There is a possibility of implant failure following ORIF surgery. This can occur due to several reasons, including mechanical stress on the implants, poor bone healing, or infection. Implant failure may require a revision surgery to replace or reposition the devices. The healthcare team will closely monitor the patient’s progress during the recovery phase to identify any signs of implant failure and take appropriate action.
Scarring
Scarring is a common outcome of surgical procedures, including ORIF surgery. The size and visibility of the scar can vary depending on various factors, such as the location and length of the incision, the patient’s individual healing process, and the surgical techniques used. While measures can be taken to minimize scarring, it is important to manage patients’ expectations regarding the potential for visible scars following ORIF surgery.

Recovery Time
Varies by Injury
The duration of recovery after ORIF surgery varies depending on the specific injury and the patient’s individual healing process. Simple fractures with minimal displacement may have a shorter recovery period compared to complex fractures involving multiple bone fragments. The surgeon will provide an estimate of the expected recovery time based on the specific case, taking into consideration factors such as age, overall health, and adherence to rehabilitation plans.
Factors Affecting Recovery
Several factors can influence the recovery time after ORIF surgery. Patient compliance with rehabilitation exercises and physical therapy can significantly impact the rate of recovery. Additionally, the presence of underlying medical conditions, such as diabetes or compromised immune function, may prolong the healing process. The nature and severity of the fracture, as well as the quality of bone tissue, can also affect the recovery time.
Expected Timeline
While the recovery timeline can vary, it is generally expected that the initial healing process will take approximately six to eight weeks after ORIF surgery. During this time, the bone fragments start to fuse together, and postoperative swelling and pain gradually subside. However, complete recovery, including regaining full strength and functionality, may take several months to a year, depending on the individual case and the recommendations of the healthcare team.
Alternative Treatments
Casting or Splinting
For some fractures, especially those with minimal displacement or in non-weight-bearing bones, alternative treatments such as casting or splinting may be considered. Casting involves immobilizing the fractured bone using a plaster or fiberglass cast, which holds the bone in place and allows for proper healing. Splinting, on the other hand, involves using a rigid or flexible device to stabilize the injury. These alternative treatments may be recommended when the fracture can be adequately aligned and stabilized without the need for surgical intervention.
External Fixation
External fixation is another alternative to ORIF surgery, particularly in cases where surgical intervention may not be feasible or necessary. This involves using external devices, such as metal pins or wires, to immobilize and realign the fractured bone. External fixation can be used as a temporary measure in situations where the patient’s condition or injury requires further assessment or when the wound cannot tolerate internal fixation devices. It is commonly used for open fractures or fractures with considerable tissue damage.
Non-Surgical Options
In some cases, non-surgical options may be considered as an alternative to ORIF. These may include non-weight-bearing restrictions, immobilization with a brace or boot, physical therapy, and pain management medications. Non-surgical options are typically reserved for fractures with minimal displacement or certain stable fractures that do not require surgical intervention. The healthcare team will assess the specific fracture and discuss the most appropriate treatment options with the patient.

Success Rate and Prognosis
Factors Influencing Success
Several factors can influence the success rate and prognosis of ORIF surgery. The severity and location of the fracture, the patient’s overall health, age, and lifestyle factors all play a role. Additionally, factors such as adherence to postoperative care instructions, rehabilitation plans, and physical therapy significantly impact the outcome. Close communication and collaboration between the patient and healthcare team are essential for ensuring the best possible prognosis.
Long-Term Outcomes
The long-term outcomes following ORIF surgery are generally favorable, with most patients experiencing significant improvement in pain, function, and overall quality of life. Successful fracture healing, restoration of joint function, and reduction of long-term complications are common outcomes. However, complete recovery can take time, and some patients may experience residual limitations or discomfort. Regular follow-up appointments and ongoing rehabilitation can help optimize long-term outcomes and minimize potential complications.
Conclusion
ORIF, or Open Reduction Internal Fixation, is a surgical procedure used to treat fractures, dislocations, birth defects, and osteoporotic fractures. The procedure aims to restore normal function and alignment by realigning and stabilizing the bones using internal fixation devices. ORIF requires proper preparation, including medical evaluation, patient counseling, medication instructions, and surgical planning.
During the procedure itself, anesthesia is administered, and an incision is made to access the fractured bone. Fracture reduction, fixation, and closure follow the incision. After surgery, the patient is moved to the recovery room, where pain management, physical therapy, and follow-up care are provided. Risks and complications associated with ORIF include infection, bleeding, nerve damage, implant failure, and scarring.
The recovery time after ORIF varies depending on the injury and individual factors. Factors affecting recovery include patient compliance, underlying conditions, and the nature of the fracture. Alternative treatments such as casting, splinting, or external fixation may be considered in certain cases. The success rate and prognosis of ORIF are generally favorable, with long-term outcomes often leading to significant improvement in pain, function, and quality of life.
In conclusion, ORIF is an effective surgical procedure that has helped numerous individuals regain their mobility and quality of life. Consultation with a healthcare professional is crucial to determine if ORIF is the most suitable treatment option for a specific injury or condition. Proper preparation, informed decision-making, and diligent postoperative care are vital for achieving the best possible outcome for patients undergoing ORIF.